- "3 out of 4 people who suffer from an autoimmune disease (such as rheumatoid arthritis, lupus and multiple sclerosis) are women" (1);
- women are 2 times more likely than men to be diagnosed with thyroid diseases (1);
- 2-3 times more likely than men to suffer depression (1);
- 2 times more likely than men to contract gallstones (1);
- more likely than men to suffer a second heart attack within the year after their first heart attack (1);
- women who smoke are up to 70% more likely to develop lung cancer than men who smoke (1);
- 80% of people affected by osteoporosis are women (1);
- women are more like to suffer migraines than men (1)
- a woman's liver metabolizes alcohol and drugs less efficiently than a man's liver (1);
- a woman's heart is one third the size of a man's heart and beats faster (1);
- woman wake up faster from anesthesia after surgery (1);
- a woman's brain is neurologically different from a man's brain (1);
- a woman's heart responds to high blood pressure by developing thicker walls which puts them at greater risk for heart failure than men (4).
Women and heart disease-
Heart disease is another area where gender based biology has identified differences between men and women. In 1991 the National Institutes of Health (NIH) implemented a landmark observational study concluded in 2006 called the Women's Health Initiative (WIN). WIN provided a great deal of data on women's health. Noteworthy is the finding that women aged 65 and older were more likely to die from heart disease than men. Also, under age 50 a woman's heart attack is twice as likely to be fatal as a man's (5). Experts suggest there are several reasons for this, one of them being that the symptoms of heart attack that men experience aren't necessarily the same for a woman (3). They can be more subtle than the severe chest pain that is the hallmark symptom for men. As a matter of fact, 71% of women reported feeling flu like symptoms in the weeks prior to having a heart attack (5). You can find more information on the topic of heart attack symptoms on The Mayo Clinic website here. A simple, noninvasive way to test for heart disease is the exercise stress test and recent research has provided more insight into the uniqueness of a woman's heart and the use of this diagnostic test.Women Take Heart Study-
The Women Take Heart Study, conducted by researchers at Northwestern University, focused on determining the normal response of a woman's heart to exercise stress testing. An exercise stress test or treadmill test is used to check a variety of heart functions including: "heart rate, breathing, blood pressure ECG, and how tired you become when exercising" (7). A stress test can also help diagnose or predict safe levels of exercise, coronary artery disease, possible causes of chest pain, and risk for heart attack (7). During a stress test doctors monitor a patient to determine if they are unable to reach at least 85% of their maximum heart rate. Failure to reach this benchmark means a greater risk of death from heart disease. How a woman's heart rate (HR), or the number of times a heart beats per minute (BPM), responded to the stress of an exercise stress test wasn't understood very well until the Women Take Heart Study. This is because up until this point most of the research in this area had been conducted on men.Maximum heart rate formula based on male data-
Scientists have known that maximal heart rate (MHR) decreases with aging (9). As a result, the formula that doctors typically use to calculate a normal response to exercise stress includes a person's age. However, the formula doesn't take into account gender differences. The simplest form of the maximal heart rate calculation based on data gathered from research using men is: Average maximal HR (MHR) = 220 - age in years (9).New maximum heart rate formula for women-
Now to the Women Take Heart study's exciting findings! This year Northwestern University researchers published results of their study that found "the traditional male-based calculation [of MHR = 220 - age] overestimates the maximum heart rate for age in women" (8) especially in women over age 35 (10). The new gender specific formula for MHR is:
MHR = 206 - 88 percent of your age
Aerobic physical activity and heart rate-
Women whose stress tests were measured using the old formula tended to show a poorer prognosis, so this gender specific formula reflects a more accurate prediction of a woman's risk for heart disease. The new formula is also important because heart rate is the standard method for monitoring aerobic exercise intensity. Using this new formula for MHR while calculating an aerobic training heart rate will more accurately reflect how hard a woman is exercising during aerobic physical activity. For example, a 50 year old woman's MHR using the old formula would be: 220 - 50 = 170. If she were shooting to work at a moderate to vigorous intensity range her training heart rate (THR) using the old MHR formula and the simple THR formula would be: 111 (170 x 65%) at the range's lower end and 145 (170 x 85%) at the range's higher end (see the Heart Rate Training Zones Chart below).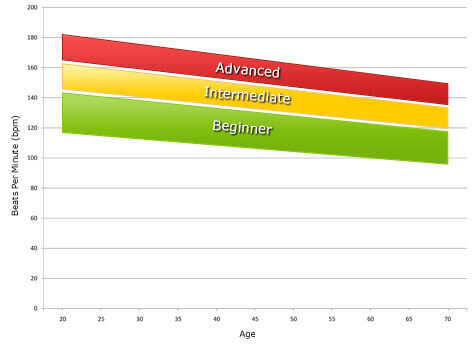 |
| From American Council on Exercise |
Using the new Women Take Heart MHR formula a 50 year old woman's MHR would be: 206 - .88(50) = 162. So, now the lower end of her THR range would be: 105 (162 x 65%) and at the higher end of her THR: 138 (162 x 85%).
Most charts will reflect training heart rate zones calculated with the old "men only" formula so keep this in mind when you're at the gym monitoring your exercise intensity. Also, exercise equipment and heart rate monitors have usually calculated THR using the old formula. However, some companies are already updating their equipment, but ask to be sure. There's also talk of an I phone app that can do the calculations for us.
It's important to note that some medications, like beta blockers taken for blood pressure control for example, can give false pulse readings. In this case, it is more accurate to measure your level of aerobic exercise intensity using Rate of Perceived Exertion or the Talk Test. You can read more about the rate of perceived exertion here, and the talk test here. Next week's post will go into a little more detail about the aerobic training zones, discuss the myth of the fat burning zone and also look at how doctors are using heart rate response to exercise as a predictor of disease and even death.
There were some limitations to the Women Take Heart study. Nevertheless, the researchers at Northwestern state that their findings "should be incorporated into clinical practice" (12). This research also underscores the importance of conducting more studies that take into consideration the fact that women are biologically unique and not just mini-men. Thanks to gender based biology research, health care might begin to treat the sexes differently.
Sources
(1) Gender Biology: Men and Women Really Are Different. Films Media Group, 1998. Films On Demand. Web. 20 November 2010. <http://digital.films.com/PortalPlaylists.aspx?aid=10103&xtid=11115>.
(2) http://www.nature.com/nm/journal/v2/n11/abs/nm1196-1248.html
(3) http://www.mayoclinic.com/health/heart-disease/HB00040
(4) http://www.washingtonlifescience.com/readlist/ceo_bianco.htm
(5) http://www.womensheart.org/content/HeartDisease/heart_disease_facts.asp, http://www.womensheart.org/content/HeartAttack/heart_attack_symptoms_risks.asp
(6) http://www.nhlbi.nih.gov/whi/
(7) http://www.heart.org/HEARTORG/Conditions/HeartAttack/SymptomsDiagnosisofHeartAttack/Non-Invasive-Tests-and-Procedures_UCM_303930_Article.jsp(8) http://www.medpagetoday.com/PrimaryCare/ExerciseFitness/20954
(9) American College of Sports Medicine, Resource Manual for Guidelines for Exercise Testing and Prescription, 2nd ed.
(10) http://seattletimes.nwsource.com/html/health/2012244688_heart05.html
(11) http://www.cdc.gov/physicalactivity/everyone/measuring/index.html(12) http://www.medpagetoday.com/PrimaryCare/ExerciseFitness/20954


it's amazing that the medical community has lagged behind using true information analysis to define these kinds of health guidelines. Good to see they are starting too. Long way to go. Great Educational post!
ReplyDelete